There is no one treatment that can cause someone to come out of a coma. Treatments can prevent further physical and neurological damage, however.
First, doctors ensure that the patient isn't in immediate danger of dying. This may require placing a tube in the patient's windpipe through the mouth, and hooking up the patient to a breathing machine, or ventilator. If there are other serious or life-threatening injuries to the rest of the body they will be dealt with in order of decreasing severity. If excess pressure in the brain caused the coma, doctors can relieve it by surgically placing a tube inside the skull and draining the fluid. A procedure called hyperventilation, which increases the rate of breathing to constrict blood vessels in the brain, can also relieve pressure. The doctor may also give the patient medication to prevent seizures. If a drug overdose or condition such as very low blood sugar is responsible for the coma, doctors attempt to correct this as soon as possible. Patients with acute ischemic strokes may undergo procedures or receive special clot-busting medication in an effort to restore blood flow to the brain.
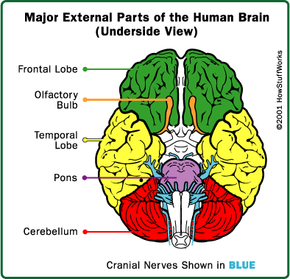
Doctors may use imaging studies, such as magnetic resonance imaging (MRI), or computed tomography (CT) scans, to look inside the brain and identify a tumor, pressure, and any signs of damage to the brain tissue. Electroencephalography (EEG) is a test used to detect any abnormalities in the brain's electrical activity. This can also show brain tumors, infections, and other conditions that might have caused the coma. If the doctor suspects an infection such as meningitis, he may perform a spinal tap to make the diagnosis. To perform this test, a doctor inserts a needle into the patient's spine and removes a sample of cerebrospinal fluid for testing.
Once the patient is stable, doctors will concentrate on keeping him or her as healthy as possible. Coma patients are susceptible to pneumonia and other infections. Many comatose patients stay in the hospital's intensive care unit (ICU), where doctors and nurses can continually monitor them. People who are in a coma for a long time may receive physical therapy to prevent long-term muscle damage. Nurses will also move them periodically to prevent bedsores -- painful skin wounds caused by lying in one position for too long.
Because patients who are in a coma can't eat or drink on their own, they receive nutrients and liquids through a vein or feeding tube so that they don't starve or dehydrate. Coma patients may also receive electrolytes -- salt and other substances that help regulate body processes.
If a coma patient continues to be dependent on a ventilator to breathe, they may receive a special tube that goes directly into their windpipe through the front of the throat (a tracheotomy). The tracheotomy tube can be left in place for extended periods of time because it requires less maintenance and does not injure the soft tissues of the oral cavity and upper throat. Because patients who are in a coma can't urinate on their own, they will have a rubber tube called a catheter inserted directly into their bladder to remove the urine.