If you've ever watched "Monty Python and the Holy Grail," chances are you have a clear mental image of what a plague-stricken village looks like. It's dirty – even squalid – and its inhabitants are similarly filthy. There's also one resident with a very particular occupation. He wheels a cart through town, calling, "Bring out your dead!" The other villagers are all too willing to comply, and some even want to add their still-living relatives to the cart.
The scene is meant to be funny, but in many ways, it's not too far off the mark. Plague is a real disease, and for much of human history, outbreaks have sparked desperate attempts to stop its spread. During past plague pandemics, some communities persecuted and executed minorities believed to be responsible for the illness. Officials also sealed infected people and their families inside their homes. People under such quarantines had no way of working or buying food, and starvation was a real possibility. Death tolls were so high that bodies had to be carted away and buried together in mass graves. Because of the sheer number of deaths in England, there is less genetic diversity there today than there was in the 11th century [source: New Scientist].
Advertisement
Body collectors and grimy villages may seem like things of the past, especially in affluent parts of the world. But in some countries, including Vietnam and India, people can still remember the most recent plague epidemics. In several parts of the world, plague is endemic – it exists all the time, but not necessarily in epidemic proportions. Today, people can contract plague in major cities as well as in more remote areas. There are a few hundred to a few thousand new cases around the world every year.
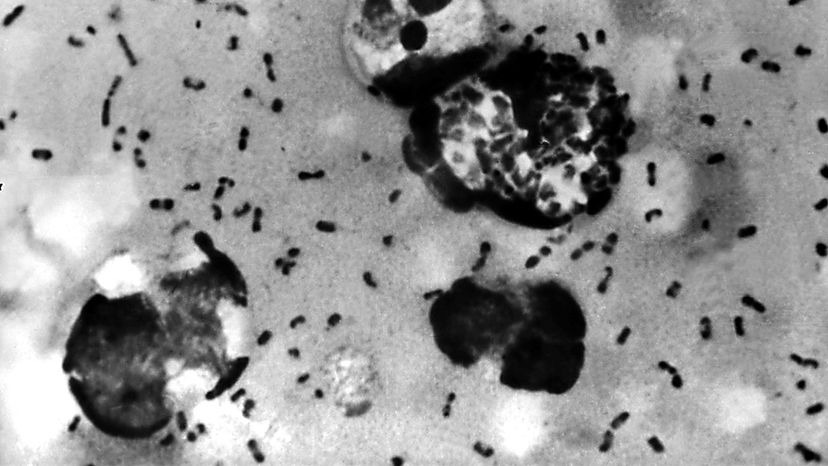
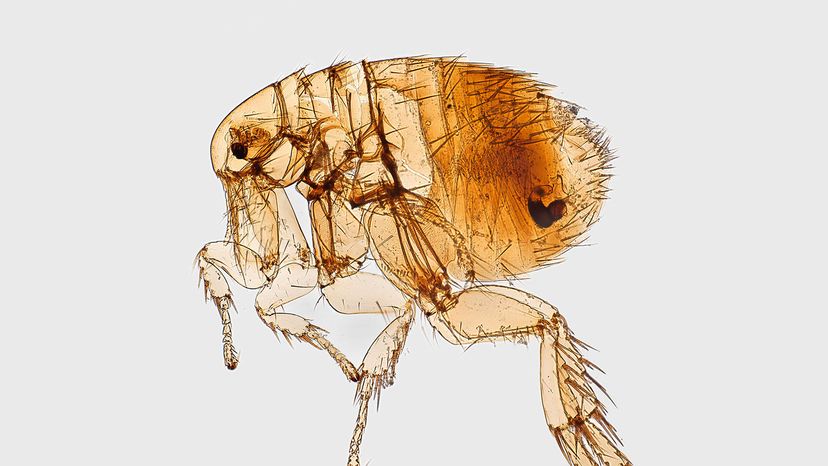
Plague is an infectious disease caused by a bacterium called Yersinia pestis. It spreads throughout animal populations, including humans, through the bites of infected fleas. These fleas often feed on rats, which is why large numbers of dead rats are a sign of an impending epidemic. The most well-known form of plague, bubonic plague, is named for the painfully swollen lymph nodes, or buboes, that the disease causes.
In this article, we'll explore how Yersinia pestis lives, reproduces and creates infections. We'll also look at plague's symptoms and how doctors can treat it. Let's begin by examining plague's history and some of the controversies behind the epidemics that have been attributed to it.
Advertisement